The Fecal Immunochemical Test (FIT) is a crucial tool in colorectal cancer screening programmes across the UK. It helps detect traces of blood in stool, which may indicate early signs of cancer or other gastrointestinal conditions. Many patients ask, “what percentage of positive FIT tests are cancer?” Knowing the statistics behind positive results can help reduce anxiety and encourage timely medical follow-up.
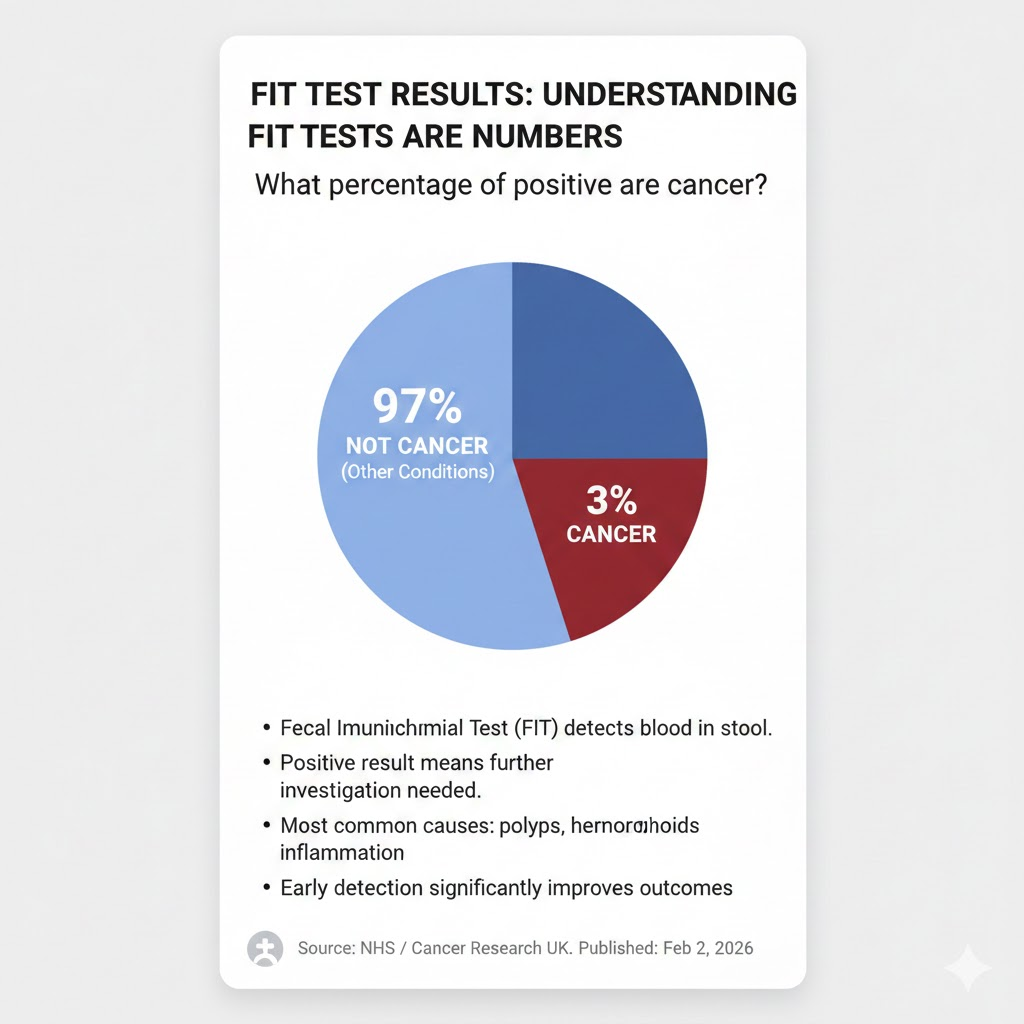
A positive FIT test does not necessarily mean cancer. Various benign conditions, such as haemorrhoids, polyps, or minor gastrointestinal bleeding, can trigger a positive result. Research suggests that the risk of a positive FIT test actually resulting in cancer ranges from 3% to 12.5%, depending on factors such as age, sex, and the level of haemoglobin detected in the stool. Understanding this percentage is vital for patients navigating their next steps.
What a Positive FIT Result Really Means
A positive FIT result is primarily a signal that further investigation is required, rather than a confirmed diagnosis. The most common follow-up is a colonoscopy, which allows healthcare professionals to identify the exact cause of bleeding and assess whether it is malignant or benign. Patients should understand that a positive test is a precautionary measure designed to detect cancer early.
Other conditions can contribute to a positive FIT result. Haemorrhoids, anal fissures, or minor intestinal bleeding often lead to detectable blood in stool without indicating cancer. By comprehending the various causes behind a positive result, patients can avoid unnecessary worry while appreciating the importance of early detection in preventing severe health outcomes.
Cancer Detection Rates in Positive FIT Results
Understanding “what percentage of positive FIT tests are cancer?” requires looking at research data and clinical studies. The detection rate varies, with most studies suggesting a risk between 3% and 12.5%. This variation is influenced by patient-specific factors such as age, sex, and personal or family history of colorectal cancer. Additionally, higher haemoglobin levels in the FIT test correlate with increased cancer risk.
This risk highlights the importance of not ignoring a positive FIT result. While the majority of positive tests do not indicate cancer, early detection through follow-up colonoscopy can significantly improve outcomes if cancer is present. Understanding these percentages empowers patients to make informed health decisions and adhere to recommended screening protocols.
Other Findings After a Positive FIT Test
Most positive FIT tests do not result in a cancer diagnosis but may reveal other health issues. Common findings include advanced adenomas, polyps, or other gastrointestinal abnormalities. Identifying these conditions early is crucial because some, if left untreated, can develop into cancer over time. FIT testing is therefore valuable not only for cancer detection but also for broader preventive healthcare.
Even when cancer is absent, treating polyps or other abnormalities can significantly reduce the risk of future malignancies. Patients often gain reassurance from understanding that “what percentage of positive FIT tests are cancer?” is relatively low, while recognising the test’s broader health benefits beyond cancer detection alone.
Reducing Anxiety After a Positive FIT Test
Receiving a positive FIT test result can be stressful, and it is normal to feel anxious while waiting for further investigation. However, understanding the actual risk of cancer helps manage this anxiety. Knowledge that only 3%–12.5% of positive results result in cancer encourages patients to take a measured approach and prioritise follow-up investigations.
Managing anxiety also involves open communication with healthcare providers. Discussing individual risk factors, lifestyle considerations, and next steps ensures clarity and reassurance. Patients should be encouraged to focus on the preventive advantages of early screening, knowing that a positive result does not automatically indicate a life-threatening condition.
Factors Affecting FIT Accuracy and Cancer Risk
Several factors can influence FIT test accuracy, including diet, medications, and pre-existing gastrointestinal conditions. These variables can occasionally lead to false positives, reinforcing the importance of careful interpretation by healthcare professionals. Awareness of these factors helps patients understand why a positive result may not always equate to cancer.
Biological factors also play a significant role. Age, gender, and medical history affect the likelihood of a positive FIT indicating cancer. The variation in detection rates explains why “what percentage of positive FIT tests are cancer?” is not a fixed figure but a range that reflects multiple individual factors and population-based studies.
Preventive Measures and Screening Recommendations
Routine FIT testing is a vital element of colorectal cancer prevention. In the UK, adults aged 60–74 are encouraged to participate in biennial screening, which can detect early signs of cancer or precancerous changes. Lifestyle factors, including a balanced diet, regular exercise, and avoiding smoking, further reduce colorectal cancer risk while complementing the benefits of screening.
The combination of regular FIT testing and healthy lifestyle choices improves early detection rates and long-term health outcomes. Understanding “what percentage of positive FIT tests are cancer?” reinforces the importance of adherence to screening schedules and proactive health management, ultimately helping to reduce the incidence and impact of colorectal cancer.
Conclusion
Knowing “what percentage of positive FIT tests are cancer?” helps patients approach their results with perspective and clarity. While the risk ranges from 3% to 12.5%, most positive tests do not indicate cancer but still require follow-up to rule out serious conditions. Timely colonoscopy, early detection, and preventive measures remain essential for long-term health and reassurance.
FAQs
What does a positive FIT test indicate?
A positive FIT test shows blood in the stool and suggests the need for further investigation, such as a colonoscopy, to determine the cause.
How likely is cancer after a positive FIT?
The risk ranges from 3% to 12.5%, influenced by age, sex, and haemoglobin levels.
Can a positive FIT test be caused by non-cancer conditions?
Yes, haemorrhoids, polyps, and minor gastrointestinal bleeding can all lead to a positive FIT result.
What is the NHS follow-up after a positive FIT test?
Patients are usually referred for a colonoscopy to identify the exact cause of bleeding.
Does a higher FIT reading mean cancer is more likely?
Higher readings increase the risk, but they do not guarantee a cancer diagnosis.
How often should I take a FIT test if I’m at average risk?
Routine FIT screening is offered every two years for people aged 60–74 in the UK.
Can lifestyle affect FIT test results?
Yes, diet, medications, and underlying health conditions can influence FIT accuracy and results.